You can’t say you haven’t been warned: there are creepy crawlies in this post


Things I will never like:
1. Drying off with a cold, damp towel.
2. The feeling of seaweed wrapping around my legs.
3. Anything that was popular in the 70’s.
4. Licorice, yam, or raisins.
5. That high-pitched screech that babies make.
6. Writhing maggots.
~Bill Watterson from It’s A Magical World: A Calvin and Hobbes Collection

A few weeks ago, I had a bit of home-made potato corn chowder left over that I added to our compost bin in our barnyard. It isn’t often that much animal protein makes its way into the bin so when I checked on the compost a few days later, I was amazed to see it teeming with fly maggots in the midst of their Thanksgiving feast. Ordinarily pictures and videos of maggots would not find their way to this blog. People might be looking at this blog while eating their breakfast or lunch and writhing maggots are not something you are expecting to see. My apologies in advance and now is the time to delete delete delete.
Therefore: a trigger warning. Don’t scroll down further if you would rather avoid seeing (and hearing) creepy crawly things.
My first medical exposure to maggots came while examining the leg and foot wounds of the homeless folks I helped care for when training in an inner city emergency room. Peeling off old ragged stockings and socks would often reveal more than dirty feet – in fact, the maggots may have been somewhat beneficial in those cases yet we were quick to dispose of them.
Maggots are, in fact, fascinating creatures with potential therapeutic value, notwithstanding their gross-out factor. This week in a brief Atlantic article found here, there is a summary of a recent study in France comparing typical surgical debridement of venous ulcers of the skin with maggot therapy. Maggots were faster in cleaning the wounds but didn’t enhance eventual healing any more than traditional surgical care. There wasn’t a difference in the discomfort level as long as the patient didn’t know which therapy was being used. For those who had been randomly assigned to maggot therapy in one study, an astounding 89% said they would opt for the insects over surgeons if faced with needing wound care in the future.
I’m not sure what that says about surgeons, but it is a great compliment to maggot larvae!
Here is a formal cross-referenced evidence-based summary from UptoDate.com about wound treatment with biologic methods:
Biologic — An additional method of wound debridement uses the larvae of the Australian sheep blow fly (Lucilia [Phaenicia] cuprina) or green bottle fly (Lucilia [Phaenicia] sericata, Medical Maggots) [42,43]. Maggot therapy can be used as a bridge between debridement procedures, or for debridement of chronic wounds when surgical debridement is not available or cannot be performed [44]. Maggot therapy may also reduce the duration of antibiotic therapy in some patients [16].
Maggot therapy has been used in the treatment of pressure ulcers [45,46], chronic venous ulceration [47-50], diabetic ulcers [42,51], and other acute and chronic wounds [52]. The larvae secrete proteolytic enzymes that liquefy necrotic tissue, which is subsequently ingested while leaving healthy tissue intact. Basic and clinical research suggests that maggot therapy has additional benefits, including antimicrobial action and stimulation of wound healing [43,47,53,54]. However, randomized trials have not found consistent reductions in the time to wound healing compared with standard wound therapy (eg, debridement, hydrogel, moist dressings) [55,56]. Maggot therapy appears to be at least equivalent to hydrogel in terms of cost [56,57].
Dressing changes include the application of a perimeter dressing and a cover dressing of mesh (chiffon) that helps direct the larvae into the wound and limits their migration (movie 1). Larvae are generally changed every 48 to 72 hours. One study that evaluated maggot therapy in chronic venous wounds found no advantage to continuing maggot therapy beyond one week [48]. Patients were randomly assigned to maggot therapy (n = 58) or conventional treatment (n = 61). The difference in the slough percentage was significantly increased in the maggot therapy group compared with the control groups at day 8 (67 versus 55 percent), but not at 15 or 30 days.
The larvae can also be applied within a prefabricated “biobag”, commercially available outside the United States, that facilitates application and dressing change [58-61]. Randomized trials comparing “free range” with “biobag”-contained larvae in the debridement of wounds have not been performed.
A main disadvantage of maggot therapy relates to negative perceptions about its use by patients and staff. One concern among patients is the possibility that the larvae can escape the dressing, although this rarely occurs. Although one study identified that approximately 50 percent of patients indicated they would prefer conventional wound therapy over maggot therapy, 89 percent of the patients randomly assigned to maggot therapy said they would undergo larval treatment again [62]. Perceived pain or discomfort with the dressings associated with maggot therapy may limit its use in approximately 20 percent of patients.

The STARZ show Outlander (a show and series of books by scientist Diana Gabaldon I thoroughly enjoy) used real maggots in the fifth season of the show when in 18th century America, wife (and surgeon) Claire successfully treats her husband Jamie’s snakebite wound with the larvae. Actress Caitriona Balfe describes her co-starring maggots in this brief video:


So there are still things to learn about medical therapies we used in the past which have been sidelined or forgotten in our push for modern treatment modalities. The days of leeches and maggots may not be over after all.
And now for video, complete with little maggotty sound effects — scroll down
Maggots in our compost bin – enjoying corn and potato chowder leftovers
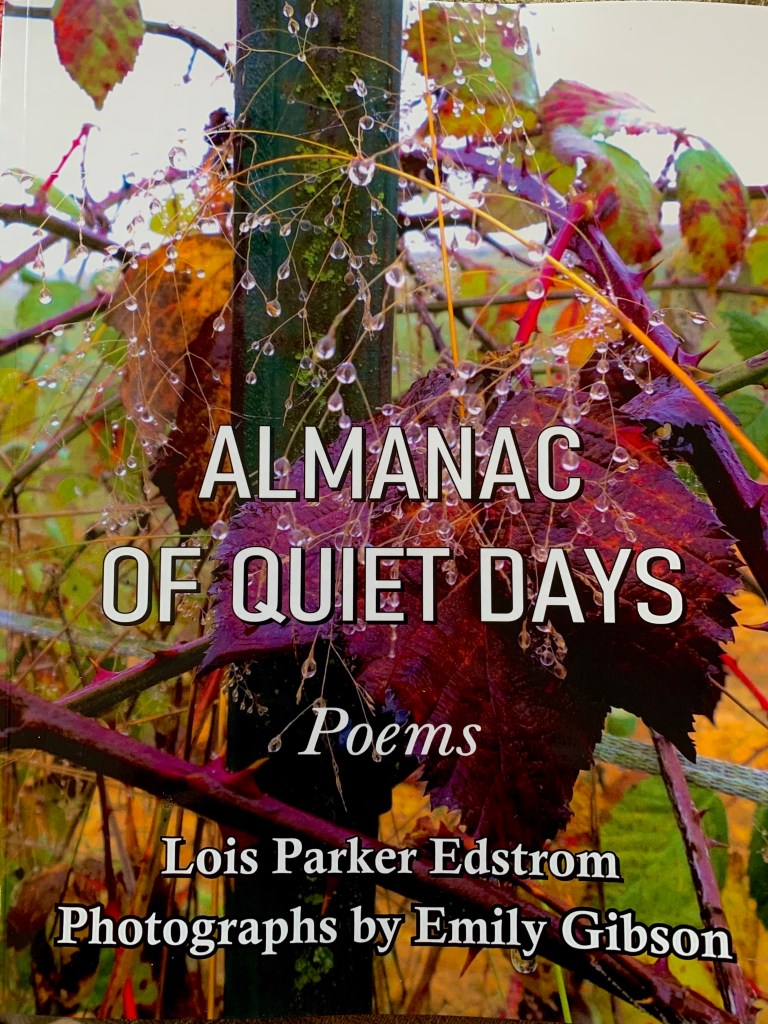
A new book from Barnstorming is available to order here
(no maggot pictures in this book, I promise!)